What is Hereditary Angioedema?
Hereditary angioedema (HAE) is a rare genetic disorder characterized by recurrent episodes of swelling (edema) of the skin in different parts of the body, as well as internal organs like the intestines or airways. The swelling is caused by increased permeability of blood vessels which leads to leakage of fluid into surrounding tissues. This results in painful, distressing and potentially life-threatening swelling attacks.
Types of HAE
There are three main types Hereditary Angioedema:
– HAE type I – accounts for 80-85% cases. It is caused by a deficiency of C1 inhibitor (C1-INH), a protein that regulates parts of the complement and contact activation systems.
– HAE type II – accounts for 15-20% cases. It is also caused by a deficiency of C1-INH but C1-INH that is produced does not function properly.
– HAE with normal C1-INH (HAE type III) – a rare form accounting for less than 5% cases. The pathogenesis is not completely understood but it is thought to involve mutations in the gene coding for factor XIIa.
Symptoms of Hereditary angioedema
The most common symptoms of HAE include:
– Recurrent episodes of severe subcutaneous or submucosal swelling affecting locations such as arms, legs, face, genitals, abdomen etc. Episodes can last 2-5 days.
– Laryngeal edema which can cause life-threatening airway obstruction and asphyxiation if not treated promptly.
– Abdominal pain and swelling caused by edema of the intestinal wall which mimics an acute surgical abdomen.
– Fatigue and malaise during and after attacks. Uncontrolled nausea and vomiting can develop during abdominal attacks.
– Symptom-free intervals may last weeks, months or years between swelling attacks.
Diagnosis of Hereditary angioedema
HAE is diagnosed based on:
– Detailed family and medical history with recurrent, unpredictable edema episodes.
– Physical exam showing non-pitting edema in the absence of hives, rashes or itching.
– Blood tests showing low levels of C1-INH for HAE types I and II. Normal C1-INH levels do not rule out HAE type III.
– Genetic testing to identify mutations in F12 or C1NH genes.
Treatment of HAE
Current treatment goals for HAE include:
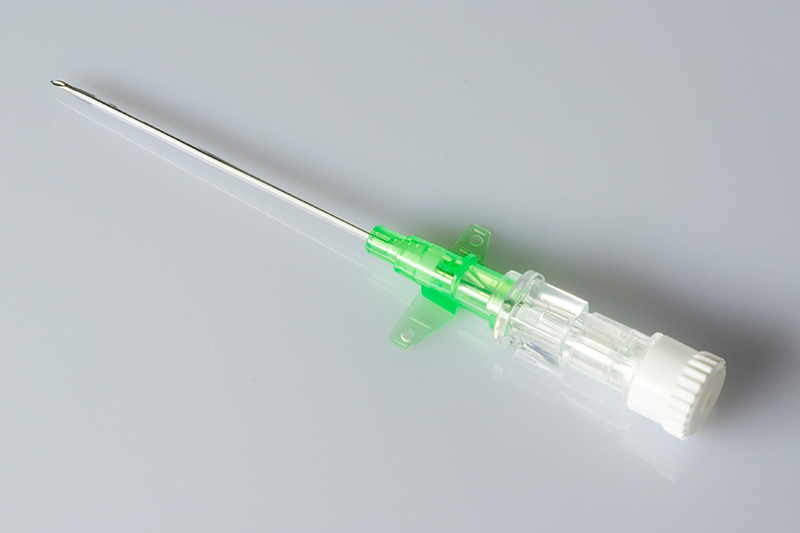
– Acute attack treatment: Intravenous or subcutaneous C1-INH concentrate or bradykinin receptor blockers like icatibant to rapidly stop swelling episodes.
– Short-term prophylaxis before procedures/surgeries: Treatment up to 3 days before and continuing after to prevent attacks.
– Long-term prophylaxis: Androgen derivatives like danazol or antifibrinolytics like tranexamic acid to reduce attack frequency.
– Attenuated androgens may cause side effects so newer options like lanadelumab are preferred.
– On-demand home therapy allows self-administration during early attacks.
– Avoid trigger factors like trauma, stress, menstrual periods for some patients.
Prognosis and Management of Hereditary angioedema
HAE can be effectively managed when diagnosed early but fatalities may occur if laryngeal attacks are untreated. Key aspects of prognosis and management include:
– Lifelong inherited condition with risk of swelling throughout life. Early detection allows prompt treatment of attacks.
– Airway compromise remains the major cause of death if emergency interventions are not instituted promptly.
– Effective prophylactic and acute therapies help minimize attacks and disability for most.
– Psychological support is advised given the unpredictable nature of swelling episodes and its impact on quality of life.
– Confirming the diagnosis prevents misdiagnosis and unnecessary surgeries or invasive procedures.
– Genetic counseling helps patients assess recurrence risk in family members.
– A multidisciplinary treatment team including immunologists, allergists, emergency physicians helps optimize long-term care.
Hereditary angioedema while a rare condition requires careful long-term management to prevent morbidity and mortality from life-threatening swelling attacks. With an established diagnosis and access to targeted therapies, patients can lead full lives with well-controlled symptoms. Further research continues to discover newer optimized treatment approaches for this complex genetic disease.