Thyroid eye disease, also known as graves’ ophthalmopathy, is an autoimmune disorder that causes inflammation and swelling of the tissues around the eyes. Left untreated, it can potentially cause serious and permanent eye damage. Fortunately, several treatment options exist to effectively manage thyroid eye disease and prevent vision loss. This article provides an overview of the various treatment approaches available.
Causes and Symptoms
Thyroid eye disease is caused by an autoimmune response where the body’s own immune system attacks the tissues surrounding the eyes. It is commonly associated with Graves’ disease, an autoimmune disorder that causes hyperthyroidism or an overactive thyroid. Common early symptoms include dry eyes, puffiness around the eyes, eyelid lag, and bulging eyes. In more advanced cases, double vision, corneal ulcerations and vision loss can occur if treatment is delayed.
Monitoring and Watching
For mild cases, doctors may recommend simple monitoring to watch for progression. This “watchful waiting” approach involves regular examinations to check for worsening symptoms. If signs remain stable over time, additional treatment may not be needed. However, patients must be carefully monitored for any changes that could signal a advancing disease.
Medications
Mild to moderate thyroid eye disease is often first treated with oral corticosteroid medications like prednisone. Corticosteroids help reduce inflammation and swelling around the eyes. Treatment usually involves taking a high dose for a short period, followed by a gradually declining dose over several months to prevent relapses. Side effects can include weight gain, mood changes and increased risk of infections.
In severe or active cases, intravenous corticosteroids may be administered in a hospital setting for short periods to rapidly decrease inflammation. Other medications options include teprotumumab, an immunotherapy drug recently approved for active thyroid eye disease. It targets the pathways driving the autoimmune response. Teprotumumab treatment requires infusions over several months but has shown significant benefits in improving symptoms and reducing the need for surgery.
Radiation Therapy
For some patients, radiation therapy may be recommended to reduce inflammation and swelling. A precision targeted form of radiation called orbital radiotherapy is delivered over a short course of 5-10 treatments. While generally well-tolerated, potential side effects include fatigue, skin irritation near the treatment area and rare cases of cataracts or dry eyes developing later. Radiation is usually reserved for cases of thyroid eye disease that do not adequately respond to medications.
Eye Muscle Surgery
In advanced stages where eye muscles and connective tissues become stretched and misaligned from swelling, eye muscle surgery may help improve double vision and appearance. The most common type is a “strabismus surgery” to align the eyes. For severe proptosis or bulging, decompression or recession surgery can be performed to move the eye back into a more protected position in the eye socket. Recovery usually takes a few weeks and glasses or patch may be required short-term after surgery.
Restoring Eyelid Position
For many patients with Thyroid Eye Disease, excess upper eyelid swelling causes the eyelids to pull down in a droopy position over the eyeballs, impairing vision. Eyelid surgery such as blepharoplasty aims to restore the normal upper eyelid position and contour. Incisions are made within the natural eyelid creases to remove excess fat and tissue and reposition the eyelids properly. Good results are usually obtained with minimal risks.
Integrating Treatment Approaches
An integrated treatment strategy tailored to the individual is most effective for thyroid eye disease. Medications are often the first-line but for some, combining medications with localized radiation or eye muscle surgery provides optimal control of signs and symptoms. Close monitoring by an ophthalmologist experienced in thyroid eye disease management allows early intervention when needed. With prompt treatment, permanent vision loss can usually be prevented, and symptoms dramatically improved in even advanced cases. Although no cure exists presently, ongoing research continues to expand options for thyroid eye related conditions.
Autoimmune Disorders and Thyroid Eye Disease
While not all patients with Graves’ disease or other thyroid conditions will develop thyroid eye disease, the link between these autoimmune conditions is clear. About 50% of people with Graves’ hyperthyroidism, the most common form of hyperthyroidism, will experience some degree of eye involvement from thyroid eye disease at some point. Women are 5-10 times more likely than men to develop both thyroid disorders and related eye issues. Other autoimmune diseases like lupus, rheumatoid arthritis and Sjögren’s are also occasionally associated with development of thyroid orbitopathy.
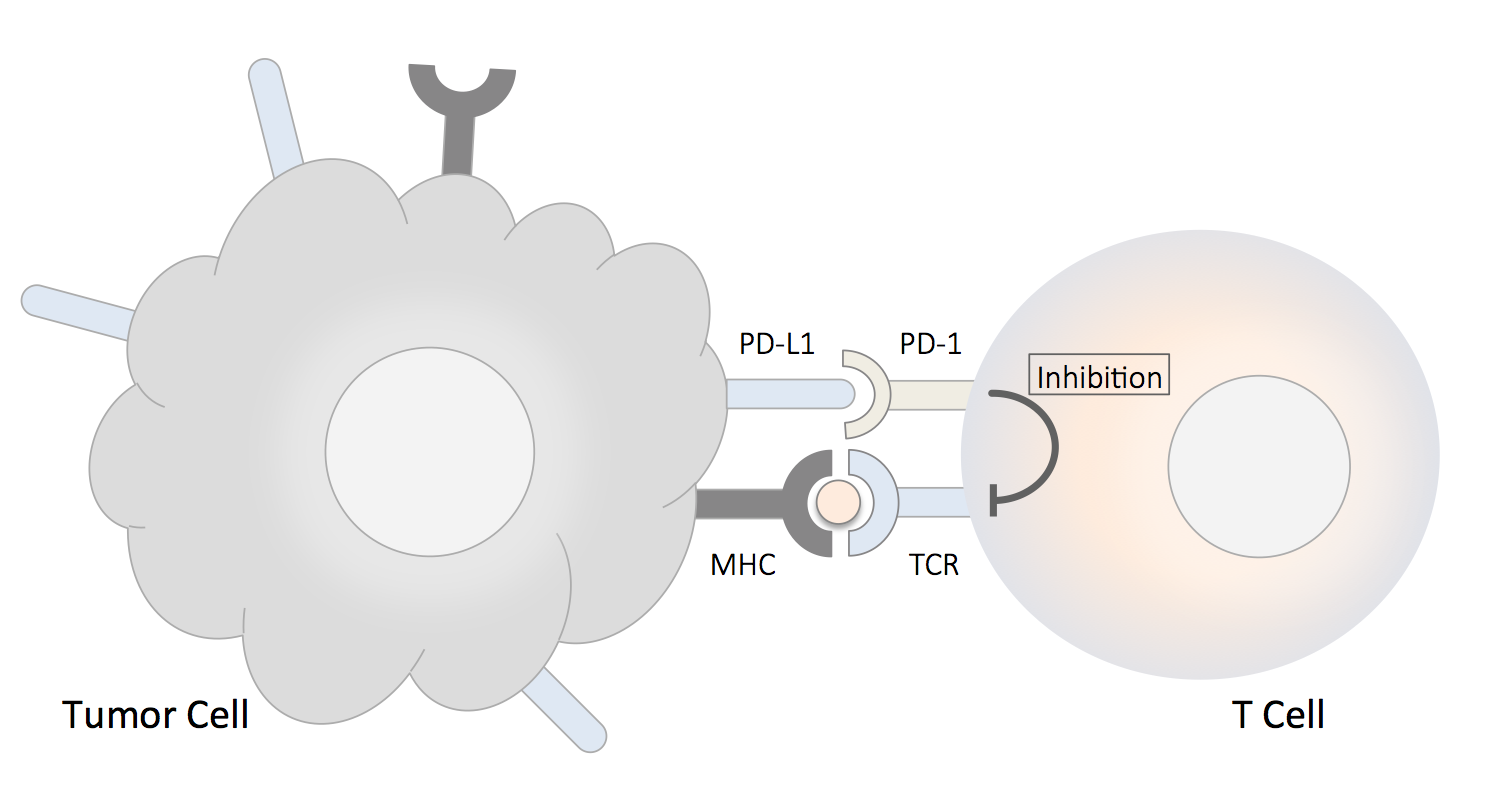
The reason for this connection is that Graves’ disease, thyroid eye disease and other autoimmune illnesses share similar aberrant autoimmune pathways driving inflammation in various tissues. In thyroid eye disease, the fibroblasts and fat tissue around eye muscles are the sites attacked due to molecular mimicry between thyroid and orbital antigens. Genetic predispositions, environmental triggers and hormonal factors are thought to contribute to unleashing these autoimmune responses in some individuals. Patients should be aware of risks and monitored closely if they have a history of autoimmune disorders to catch eye disease early on.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it